Vaginal discharge(LEUCORRHEA) is the most common gynaecological condition encountered by physicians. Normal secretion or discharge from the vagina is white and odourless and collects in the dependent part of vagina (posterior fornix). The normal Ph of vagina is 3.8 – 4.5 and the normal vaginal flora are Aerobic bacteria like Lactobacilli, Streptococcus, Staphylococcus and Gardnerellavaginalis, whereas Anaerobic bacteria are Peptococcus, Peptostreptococcus and Bacterioids.
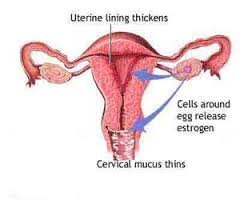
Pathophysiology may be Physiological or pathological. The vaginal epithelium is sensitive to hormonal changes during menstrual cycle. Under influence of oestrogen, maturation and keratinization of cells occur. With the effect of oestrogen, superficial cells produce glycogen which converts to lactic acid by lactobacilli. The pH of vagina is therefore acidic. Along with acidic Ph and hydrogen peroxide produced by lactobacilli protects against bacterial infections. Whereas in postmenopausal and prepubertal state, due to absence of oestrogen, the glycogen content is low, pH turns alkaline and epithelium is non keratinized and thin, therefore susceptibility to infection is more.
Physiological leucorrhea:This physiologic discharge is formed by mucoidendocervical secretions in combination with sloughing epithelial cells, normal vaginal flora and vaginal transudate. This may increase in secretions during ovulation, premenstrually or on use of estrogen-progestin contraceptives and during pregnancy. Diet sexual activity, medications and stress can also affect the volume and character of normal vaginal discharge.The discharge is mucoid, has no odour and non-irritant.
Pathological Leucorrhea:Pathological discharge may be from leisions in the vagina, cervix, or due to pelvic inflammatory disease(PID). The aetiology varies in different age groups. In children, it is commonly due to vulvovaginitis, in women of reproductive age group, it is due to vaginitis, cervicitis or PID. In menopausal women, malignancy must be ruled out.
VAGINAL DISCHARGE IN CHILDREN:Prepubertaloestrogen deficiency increase the susceptibility of vagina to infections. The causes may be non-specific vulvovaginitis or specific vulvovaginitis. Among nonspecific type it might be due to poor hygiene, allergy and foreign body. Whereas in specific vulvovaginitis type it may be due to streptococci, pinworm, candida, trichomonas and other bacteria.
VAGINAL DISCHARGE IN REPRODUCTIVE AGE GROUP: The causes of vaginal discharge in reproductive women are mainly vaginitis, cervicitis, acute pelvic infection and chronic pelvic infection.
Vaginitis is the most common cause of vaginal discharge. Mainly due to Bacterial vaginosis, Thrichomonas vaginitis and Candida vaginitis.
BACTERIAL VAGINOSIS: This is the most common vaginal infection. There is increase in anaerobic bacteria including G.Vaginalis, Prevotella and Mobiluncus species. Multiple sexual partners is a risk factor, Hence it is not sexually transmitted disease but a sexually associated disease. Clinically the discharge is white in colour, thin homogenous liquid with a fishy odour (characteristic). Bacterial vaginosis increases the risk for pelvic inflammatory disease, postoperative and postabortal infections, and obstetric complications like preterm labour and premature rupture of membranes. Recurrent infections are common. The criteria to diagnose bacterial vaginosis is “AMSELS CRITERIA”. Three out of four of the criteria should be present for making a diagnosis.
The criteria includes:
- Homogenous vaginal discharge
- vaginal PH more than or equal to 4.5,
- amine-like odour on addition of KOH (whiff test)
- Clue cells on wet smear.
The treatment of bacterial vaginosis is metronidazole 400mg twice daily for seven days or clindamycin 300 mg twice daily for seven days.
TRICHOMANS VAGINITIS:This infection is caused by the protozoan Trichomonasvaginalis. It is a highly contagious sexually transmitted disease. The discharge is yellow in colour frothy appearance associated with foul odour. The vagina is usually inflamed and oedematous with typical “STRAWBERRY” appearance named as “strawberry vagina”. There may be associated soarness of the vulva, perineum and thighs. Diagnosis is made by wet smear examination of the discharge, which reveals motile flagellated organisms. The infection can coexist with bacterial vaginosis. In pregnant women it can cause premature rupture of membranes and preterm labour. Management includes metronidazole 400mg twice daily orally for seven days or tinidazole 1gram single dose orally.
CANDIDA VAGINITIS:The organism causing iscandida albicans, is a part of normal vaginal flora and causes 90% of candida vaginitis.
The risk factors for candida are:
- Pregnancy
- Oral contraceptive use
- Menstruation
- Antibiotic use
- Obesity
- Diabetes
- Immunosuppression like corticosteroids, HIV infection and Immunosuppressive drugs
The main clinical symptom is thick curdy white discharge and tends to adhere to the vaginal wall forming plaques, with no odour along with pruritis. The vulval skin is usually involved as well with erythema, excoriation, edema and dysuria. In contrast to other types of vaginitis the pH is less than 4.5 in candida. The diagnosis can be made on identification of pseudohyphae, hyphae and spores on addition of KOH. However the treatment can be initiated on the basis of clinical diagnosis.
The treatment is based on severity. In uncomplicated infection clotrimazole 100mg twice daily for three days, whereas in oral candidiasis fluconazole 150mg single dose can be given, as in complicated infection, Intravaginal or oral fluconazole 150mg two doses 72 hours apart is adviced.
About 3-5% of women develop recurrent infections, culture is required to confirm the diagnosis, identify the fungal species and determine sensitivity. Oral fluconazole 150mg every three days for nine days followed by weekly for six months.