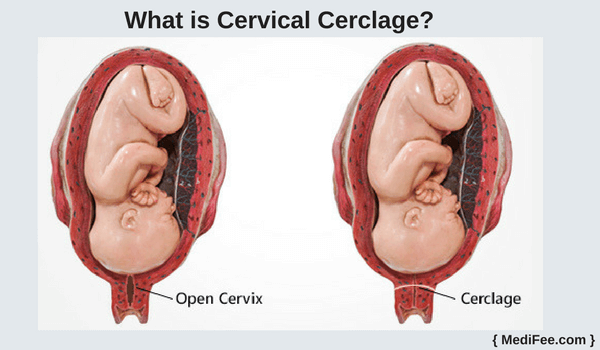
Cervical insufficiency is an important cause of preterm birth and is estimated to complicate up to 1% of pregnancies . A cerclage, or purse-string suture around the cervix, can be used to treat cervical insufficiency and prevent second-trimester loss and preterm birth. Traditionally, a cerclage is placed vaginally, a cerclage may be instead placed abdominally in more severe cases where a vaginal cerclage has failed or the cervix is extremely short. An abdominal cerclage allows for placement of the suture at the internal os, providing greater structural support to the cervix. The absence of a foreign body in the vagina may also reduce the risk of ascending infection and resulting preterm labor or ruptured membranes . Despite these advantages, an abdominal cerclage is rarely the first-line treatment for cervical insufficiency because it necessitates a cesarean delivery. The procedure is also viewed as a more morbid option due to the risk of bleeding from the uterine vessels
and traditional reliance on laparotomy for placement. Increasingly, an abdominal cerclage is placed laparoscopically, often as a prophylactic surgery before conception. High rates of success in preventing preterm birth are reported for both the open and laparoscopic approaches, with laparoscopy offering the advantages of minimally invasive surgery . Slightly improved neonatal
survival rates with the laparoscopic method compared with an open one is also reported.
Indications for abdominal cerclage
A vaginal cerclage is indicated in patients with a history of cervical deficiency as guided by history, physical examination, or ultrasound findings. A history of cervical insufficiency is suggested by one or more second-trimester losses related to painless cervical dilation in the absence of labor or placental abruption. The findings considered to be concerning for cervical insufficiency include examination, evidence of painless cervical dilation in the second trimester or ultrasound evidence of a cervical length of <25 mm in a patient with a history of preterm birth before 34 weeks of gestation .When an ultrasound-indicated vaginal cerclage is placed, preterm delivery before 35 weeks of gestation has been shown to be reduced from 41% to 28% . For the subset of patients who have a very early spontaneous preterm delivery despite a vaginal cerclage, an abdominal cerclage may be of benefit. An abdominal cerclage has therefore typically been offered to patients who have had at least two prior failed vaginal cerclages. The open procedure is also more commonly performed after conception. Increasingly an abdominal cerclage is being offered after only one prior failed vaginal cerclage, given the ability to place the cerclage laparoscopically with a shorter recovery and fewer complications. An abdominal cerclage is more effective treatment than repeated vaginal cerclage in patients with one prior failed vaginal cerclage. Other indications for an abdominal cerclage include extreme cervical shortening or cervical deformity that is suspected to compromise the cervix. This may be the result of congenital anomalies, cervical laceration, recurrent loop electrosurgicalxcision procedures, cervical conization, or trachelectomy.
An abdominal cerclage performed for these indications is considered prophylactic.
Laparoscopic approach The obvious advantages of laparoscopic abdominal cerclage relate to the minimally invasive nature of the procedure. The laparoscopic approach is favored for many procedures given reduced blood loss, fewer wound complications, a shorter length of stay, and a faster return to normal activities compared with an open procedure. Laparoscopy lends improved visualization of the pelvic anatomy, aiding in avoidance of uterine vessel injury, a feared complication of abdominal cerclage. Many patients with cervical insufficiency have also had one or more cesarean deliveries, resulting in uterine adhesions that may be more carefully lysed with the laparoscopic method. Additionally, most patients can be discharged home the same or next day after laparoscopic abdominal cerclage.
Laparoscopic cerclage before versus after conception Laparoscopic cerclage can be placed before conception or during early pregnancy, typically before 14 to 16 weeks of gestation. Laparoscopic abdominal cerclage is often performed before pregnancy when the uterus is normal in size and there is no risk of miscarriage. The less invasive nature of laparoscopic abdominal cerclage is also more appealing as a preventative measure when a future pregnancy is not guaranteed. A systematic review found that
71% of laparoscopic abdominal cerclages are placed before conception compared with only 19% of open abdominal cerclages . The open approach may be more common during early pregnancy to help overcome the challenges of inserting the cerclage in the setting of a gravid uterus. No differences in the rate of third-trimester delivery or live birth were found between the preconception and postconception groups for either surgical approach. One study compared preconception versus postconception cerclage with the results favoring preconception insertion. Both groups had a prior midtrimester loss and at
least one prior failed vaginal cerclage. Delivery at after 34 weeks of gestation was statistically significantly higher in the preconception group compared with the postconception group.No surgical complications occurred in the preconception cerclage group whereas (5%) in the first- trimester group had a surgical complication (bladder and bowel injury) and (50%) had an estimated blood loss >500 mL.
Additionally, postconception cerclage carries a unique risk of fetal demise or miscarriage, estimated to occur in 1.2% of laparoscopic cases . Preconception cerclage is not thought to impair fertility, with 78% of laparoscopic cases achieving a future pregnancy. Most have concluded that preconception placement is
associated with reduced surgical and obstetric risk.
Cerclage in twin pregnancy Advantages
Dilated cervix ≥1 cm before 24 weeks associated with
longer latency period
Decreased incidence of spontaneous preterm birth
Improved perinatal outcomes compared to expectant
management
Disadvantage
Not ACOG Recommended
Increase risk of preterm birth
Not effective in prolonging gestation or improving fetal
outcomes
Dr Surya