Definition:
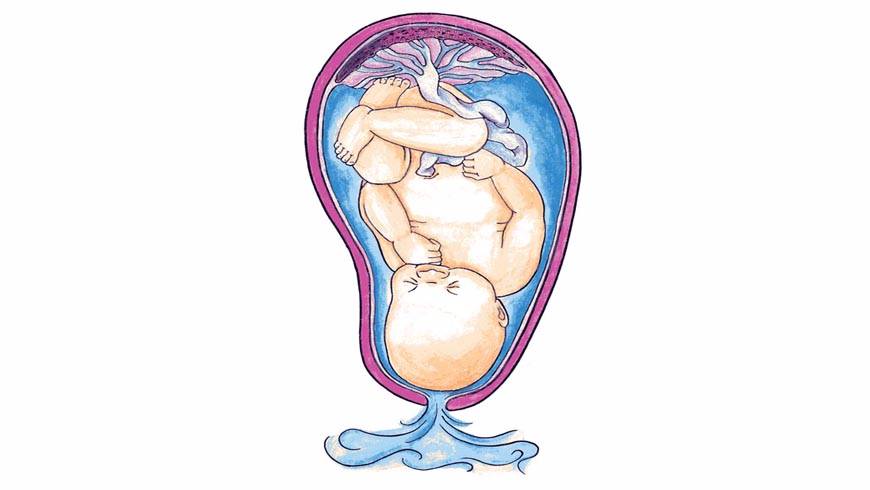
Spontaneous rupture of the membranes which happens after 28 weeks of gestational age but before theonset of labor is said to be prelabor rupture of the membranes (PROM). When rupture of membranes occur beyond37th week but before the onset of labor, it is called term PROM and when it occurs before 37 completed weeks,it is called preterm PROM. Rupture of membranes for > 24 hours before delivery is said to beprolonged rupture ofmembranes.
Incidence:
PROM occurs in approximately 10% of all pregnancies.
Causes :
In majority, the etiology is unknown. The possible causes are:
(1) Increased friability of the membranes;
(2) Decreased tensile strength of the membranes;
(3) Polyhydramnios;
(4) Cervical incompetence;
(5) Multiplepregnancy;
(6) Infection—Chorioamnionitis, urinary tract infection and lower genital tract infection; (7) Cervicallength< 2.5 cm;
(8) Prior preterm labor and
(9) Low BMI (< 19 kg/m2).
Diagnosis:
The symptom is leakage of watery discharge per vaginum either in the form of a gushor slow leak. This is often confused with :
(a) Hydrorrheagravidarum—a state where periodic watery dischargeoccurs probably due to excessive decidual glandular secretion;
(b) Incontinence of urine especially in later months.
Confirmation of diagnosis:
(1) Speculum examination is done to check the liquor leaking out through the cervix.
(2) To examine the collected fluid from the posterior fornix (vaginal pool) :
(a) Detection of pH by litmus or Nitrazine paper. The pH becomes 6–6.2 (Normal vaginal pH during pregnancy is4.5–5.5 whereas that of liquor amniis 7–7.5). Nitrazine paper turns from yellow to blue at pH > 6;
(b) To note thecharacteristic ferning pattern when a smeared slide is examined under microscope;
(c) Centrifuged cells stainedwith 0.1% Nile blue sulfate showing orange blue coloration of the cells (exfoliated fat containing cells from sebaceousglands of the fetus);
(3) AmniSure—A rapid immunoassay is accurate;
(4) Ultrasonography is to confirm the diagnosis and to assess the fetal well being.
Investigations:
(1) complete blood count;
(2) C-reactive protein (CRP);
(3) Urine for routine analysis and culture;
(4) High vaginal swab for culture (specially for Gr. B Streptococcus);
(5) Vaginal pool for estimation of phosphatidylglycerol and L: S ratio;
(6) Ultrasonography for fetal biophysical profile
(7) Cardiotocography for nonstresstest .
Dangers:
The risk less when the rupture happens near term than earlier in pregnancy.
(1) In term PROM labor starts in 80–90% of cases within 24 hours. PROM is one of the important causes of pretermlabor and prematurity;
(2) Chance of ascending infection is more if labor fails to start within 24 hours. Liquor getsinfected (chorioamnionitis) and fetal infection supervenes;
(3) Cord prolapse ;
(4) Continuous escape of liquor for long duration may lead to dry labor;
(5) Placental abruption;
(6) Fetal pulmonary hypoplasia, especially in preterm PROM is a real threat when associated with oligohydramnios;
(7) Neonatal sepsis, RDS, Intraventricular hemorrhage and Necrotizingentercolitis in preterm PROM;
(8) Perinatal morbidities (cerebral palsy) are high.
Maternal complications of PROM: Chorioamnionitis, placental abruption, retained placenta, endometritis,maternal sepsis and even death.
Management
- Aseptic examination with a sterile speculum is done not only to confirm the diagnosis but alsoto note the state of the cervix and to detect any cord prolapse;
- Patient is put to bed rest and sterile vulval pad is applied to observe any further leakage. when diagnosis isconfirmed, management depends on—
- Gestational age of the fetus;
- Check the patient is in labor or not;
- Evidence of sepsis and
- Prospect of fetal survival in that institution, if delivery occurs. Maternal pulse,temperature and fetal heart rate are monitored 4 hourly.
Term PROM : If the patient is not in labor and there is no evidence of infection or fetal distress, she is observedcarefully in the hospital. Generally in 90% of cases spontaneous labor ensue within 24 hours. If labor does not startwithin the stipulated time or there are reasons not to wait, induction of labor with oxytocin is commenced forthwith.
Cesarean section is performed with obstetric indications.
Preterm PROM:
- The main concern is to balance the risk of infection in management versus the risk of prematurity in active intervention. Ideally the patient should be transferred with the“fetus in utero” to an unit able to manage preterm neonates effectively.
- If the gestational age is 34 weeks or more, perinatal mortality from prematurity is less compared to infection(GBS). Labor generally starts spontaneously within 48 hours, otherwise induction with oxytocin is instituted.
- Presentation other than cephalic merits cesarean section. When gestational age is less than 34 weeks, conservativemanagement generally followed in absence of any maternal or fetalindications.on rare cases with bed rest, the leakseals spontaneously and pregnancy continues.
use of antibiotics:
- Prophylactic antibiotics are given to minimize maternal and perinatal risks of infection.
- Pelvic rest and antibiotics help to seal the leak spontaneously and reduce infection.
- Use of corticosteroids to stimulate surfactant synthesis against RDS in preterm neonates is advised. As suchPROM alone may accelerate fetal lung maturation. However, combined use of antibiotics and corticosteroids has reduced the risks of neonatal RDS, IVH and NEC, BPD and PDA .