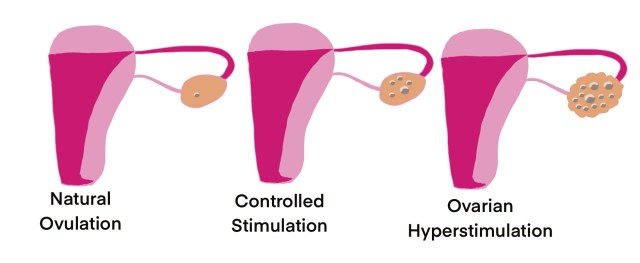
Ovarian hyperstimulation syndrome (OHSS) is an iatrogenic complication of ovarian stimulation by assisted reproductive techniques and other infertility treatments. This involves ovarian enlargement in multiple cystic forms and mainly fluid shift from the intravascular to third space of extravascular space due to increased capillary permeability and ovarian agenesis. It is mainly dependent on administration of human chorionic gonadotrophin(hCG). OHSS has been recognized in two clinical forms.
CLINICAL FORMS:
1.THE EARLY ONSET: This form occurs within first eight days after ovulation triggering injection of (Human chorionic Gonadotrophin)HCG administration.
2.THE LATE ONSET: This form occurs from ten days after HCG administration, mainly due to secretion of placental hCG
CLASSIFICTION: OHSS has been classified into grades according to severity.
MILD OHSS:
Grade1: Abdominal distension and discomfort
Grade 2: Grade 1 along with nausea, vomitingand/or diarrhea. Enlarged ovaries from 5- 12cm
MODERATE OHSS:
Grade 3: Ultrasound evidence of ascites along with mild OHSS
SEVERE OHSS:
Grade 4: Clinical evidence of ascites and/or hydrothorax and breathing difficulties along with moderate OHSS.
Grade 5: Grade 4 plus haemoconcentration, increase in blood viscosity, coagulation abnormalities and diminished renal perfusion.
PREDICTION:
- The primary risk factors include young age, a history of increased response to gonadotrophins, previous OHSS and polycystic ovarian syndrome.
- The secondary risk factors includes absolute levels of serum E2, increase in follicular size and number and number of oocytes collected.
CLINICAL FEATUTRES:
- Includes Abdominal pain, nausea and vomiting occurred due to enlargement of ovaries. Increased intra-abdominal pressure due to ascites leads to abdominal discomfort.
- Dyspnea
- Hypotension/ Hypovolemia
- Acute Renal Failure
- Electrolyte Imbalance
- Hypercoaguability
MANAGEMENT: Treatment for OHSS is based on the degree of hyperstimulation.
a). MILD HYPERSTIMULATION: It is mostly supportive, may worsen as moderate and severe form of disease. Therefore close monitoring of abdominal girth, acute weight gain and abdominal discomfort on daily basis for atleast 2 weeks.
b). MODERATE HYPERSTIMULATION: This consists of observation, bed rest, adequate fluid intake and ultrasonographic monitoring of size of cysts. Evaluation of haemogram, electrolytes and creatinine levels.Monitoring of intake and output of the fluid levels, whereas discrepancy of more than 1000ml/day of fluids is crucial sign of progression to severe form of syndrome.
c). SEVERE HYPERSTIMULATION: One should manage the patient in teritiary care centre as experienced physicians are required. Severe form of OHSS is not common, but it is dangerous. The main interventions are daily physical examination, bed rest, fluid management and correction of hypovolemia. Immediate intravenous administration of normal and /or 5%dextrose infused at the rate of 125-150ml per hour. Patient should be closely monitored for any clinical signs of overhydration. Low urine output is an indication of 200ml of 25% human albumin. Subcutaneous heparin of 5000-7500U/d to be administered to prevent thrombosis. Ultrasound guided paracentesis is indicated to manage ascites causing abdominal discomfort and pulmonary or renal compromise.
d). CRITICAL HYPERSTIMULATION: It includes liver failure, renal failure, ARDS, thromboembolic disorder and multiorgan failures. Management requires intensive care in critical care unit.
OHSS is a self-limiting disease. Therefore treatment can be mostly conservative. Medical therapy would be sufficient for most patients. Complete resolution takes 10-14 days from onset of initial symptoms. Surgery is required only in critical cases whereas ovarian torsion, ruptured cyst and internal hemorrhage.
MEDICATIONS:
Anticoagulants like heparin given at 5000-7500 units subcutaneously (SC) twice daily by preventing the activity of antithrombin III and prevents conversion of fibrinogen to fibrin and inhibits further thrombogenesis and fibrinolysis. The prognosis is excellent in mild or moderate OHSS.
PREVENTION MEASURES:
- Low-dose gonadotrophin protocols is used to stimulate the ovaries without exceeding the follicle stimulating hormone(FSH) threshold, thus facilitates the development of only few dominant follicles than multiple follicles.
- Coasting (“soft landing”) includes withholding gonadotrophin administration for atleast three or more days may decrease the risk of OHSS without modifying the pregnancy rate. However, withholding for four or more days associated with lower implantation rate.
- Modification of ovulation triggering agent: lowering the doses of hCG below 10,000 IU usually may cause sufficient oocyte maturation while reducing the risk of ovarian hyperstimulation syndrome. Replacement of hCG by exogenous or endogenous LH as ovulation trigger could have considerable impact on early form of OHSS. An endogenous LH surge can be provoked by administration of a short-acting GnRH agonist.
- Adminstration of macromolecules like intravenous administration of albumin at the time of oocyte collection has a preventive effect in cycles with a severe risk for OHSS. However albumin administration also has the side effects like viral transmission, nausea, vomiting and allergic reactions. Whereas albumin is expensive too.
- Cryopreservation of all embryos. Whereas this does not exclude the risk for early form of OHSS. The removal of a large number of granulosa cells from the follicles probably also decreases the risk of ovarian hyperstimulation syndrome.
- Avoidnace of hCG in luteal phase support(LPS) is also known to decrease the risk of OHSS.
- Insulin-sensitizing agents like metformin has crucial role in ovarian dysfunction and hyperandrogenismassociated with PCOS.
- Dopamine agonist agents like cabergolin inhibits the VEGF receptor 2 phosphorylation levels and associated vascular permeability without affecting luteal angiogenesis.
- Nonsteroidal anti-inflammatory drugs like low-dose aspirin was associated with decrease the risk of OHSS incidence.