Both fallopian tubes are involved in most (>90%) women in FGTB and the involvement can be TB endosalpingitis, exosalpingitis, interstitial TB salpingitis and Salpingitis isthmica nodosa. In tuberculous endosalpingitis, with the haematogenous route of spread, the infection starts from endosalpinx making tubes swollen, oedematous and irregular with the formation of hydrosalpinx, pyosalpinx, tubo-ovarian masses and dense adhesions. Endosalpinx may be hyperplastic or edematous or totally destroyed by disease making women more susceptible to ectopic pregnancy and infertility. In tuberculous exosalpingitis, infection starts in the muscularis mucosa of oviducts with hyperaemia, flimsy adhesions and miliary tubercles on the surface of the tubes. Later beading, closed tubes, tubo-ovarian masses, hydrosalpinx, pyosalpinx and the development of synechiae formation occurs.
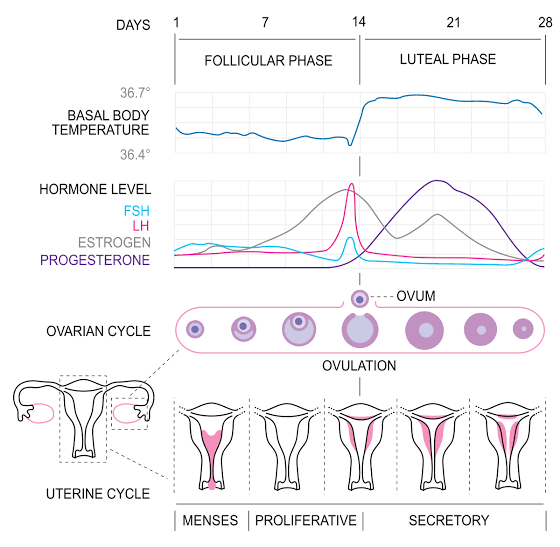
Menstruation– the recurring monthly series of physiological changes in women, which is bleeding from the vagina that happens about once a month, menstruation (also termed period or bleeding) is the process in a woman of discharging (through the vagina) blood and other materials from the lining of the uterus at about once monthly interval from puberty until menopause (ceasing of regular menstrual cycles), except during pregnancy. This discharging process lasts about 3-8 days. A menstrual cycle starts with the first day of the period and ends with the start of the next period. An entire menstrual cycle usually lasts between 24 and 38 days, but the length may vary from cycle to cycle, and may also change over the years. Cycle length changes between menarche (when periods first start during puberty) and menopause (when periods stop permanently).
The menstrual cycle is actually made up of two cycles that interact and overlap—one happening in the ovaries and one in the uterus.
1. OVARIAN CYCLE: Regular cyclic growth of follicles and release of egg each month
2. UTERINE CYCLE: Regular cyclic growth of the endometrium and shedding
There are two main hormones- estrogen and progesterone, which is responsible for this menstrual cycle to occur regularly.
The hypothalamic-pituitary-ovarian axis secretes hormones estrogen and progesterone.
Hypothalamus: located at the base of the brain, just above the brainstem. Along with homeostasis, the hypothalamus also secretes certain hormones, including gonadotropin-releasing hormone (GnRH).
Pituitary gland: it is located below the hypothalamus, in the base of the skull. This gland secretes a variety of hormones, including a follicle-stimulating hormone (FSH) and a luteinizing hormone (LH).
Ovary: the two ovaries located in a woman’s pelvis secrete estrogen and progesterone.
At the end of the menstrual cycle, the progesterone level drops. That leads to negative feedback stimulation of the hypothalamus. The hypothalamus secretes GnRH, which will initiate FSH secretion by the pituitary gland.
FSH causes the primordial follicle to mature by acting on the granulosa cells and causing their proliferation. The granulosa cells divide, and the primordial follicle changes to the primary follicle. Around 5-6 follicles mature in the ovary under the FSH’s influence each month.
Granulosa cells produce estrogen, which acts on the uterine endometrium. Estrogen causes the proliferation of endometrial stroma and the development of endometrial glands.
The glandular tissues in the fallopian tube proliferate and increase in the number of ciliated epithelial cells. The cilia become more active and propel the ovulated egg towards the uterus to maximize the chances of fertilization. Only one of the maturing follicles is able to dominate over the others. It is called the Graafian follicle. The increasing estrogen level in the blood suppresses the FSH produced by the negative feedback mechanism. The decreasing level of FSH stimulates the pituitary gland to produce LH.
LH acts on the theca cells and is required for ovulation. The increasing estrogen level will cause a surge in the LH level by the positive feedback mechanism. This phase of the reproductive cycle, from FHS release until ovulation, is called the follicular phase.
After ovulation has occurred, the ruptured follicle becomes the corpus luteum. In addition to producing estrogen, it produces progesterone. Progesterone induces the uterine endometrium’s secretory functions and signals the hypothalamus to stop producing GnRH. This, in turn, deactivates FSH and LH production.
In the initial three months of pregnancy, the corpus luteum produces progesterone, bringing the negative feedback into effect. As the pregnancy progresses, the placenta starts producing ovarian hormones to sustain the pregnancy.
The first part of the cycle
From the time bleeding starts to the time it ends, Old blood and tissue from inside the uterus is shed through the vagina. Each menstrual cycle starts with menstruation (the period). A period is the normal shedding of blood and endometrium (the lining of the uterus) through the cervix and vagina. A normal period may last up to 8 days, but on average lasts about 5 or 6.
Ovaries -Follicular phase
From the start of the period until ovulation What: Signals from the brain tell the ovaries to prepare an egg that will be released During this period, the pituitary gland (a small area at the base of the brain that makes hormones) produces a hormone called follicle stimulating hormone (FSH). FSH tells the ovaries to prepare an egg for ovulation (release of an egg from the ovary). Throughout the menstrual cycle, there are multiple follicles (fluid filled sacs containing eggs) in each ovary at different stages of developmen. About halfway through the follicular phase (just as the period is ending) one follicle in one of the ovaries is the largest of all the follicles at about 1 cm (0.4 in). This follicle becomes the dominant follicle and is the one prepared to be released at ovulation. The dominant follicle produces estrogen as it grows, which peaks just before ovulation happens. For most people, the follicular phase lasts 10-22 days, but this can vary from cycle-to-cycle.
Uterus:
Proliferative phase From the end of the period until ovulation, The uterus builds up a thick inner lining While the ovaries are working on developing the egg-containing follicles, the uterus is responding to the estrogen produced by the follicles, rebuilding the lining that was just shed during the last period. This is called the proliferative phase because the endometrium (the lining of the uterus) becomes thicker. The endometrium is thinnest during the period, and thickens throughout this phase until ovulation occurs. The uterus does this to create a place where a potential fertilized egg can implant and grow.
Ovulation:
About midway through the cycle, but this can change cycle-to-cycle. Ovulation divides the two phases of the ovarian cycle (the follicular phase and the luteal phase). An egg is released from the ovary into the fallopian tube
The dominant follicle in the ovary produces more and more estrogen as it grows larger. The dominant follicle reaches about 2 cm (0.8 in)—but can be up to 3 cm—at its largest right before ovulation. When estrogen levels are high enough, they signal to the brain causing a dramatic increase in luteinizing hormone (LH). This spike is what causes ovulation (release of the egg from the ovary) to occur. Ovulation usually happens about 13-15 days before the start of the next period.
The second part of the cycle Ovary:
Luteal Phase
From ovulation until the start of the next period. The sac that contained the egg produces estrogen and progesterone. Once ovulation occurs, the follicle that contained the egg transforms into something called a corpus luteum and begins to produce progesterone as well as estrogen. Progesterone levels peak about halfway through this phase. The hormonal changes of the luteal phase are associated with common premenstrual symptoms that many people experience, such as mood changes, headaches, acne, bloating, and breast tenderness. If an egg is fertilized, progesterone from the corpus luteum supports the early pregnancy. If no fertilization occurs, the corpus luteum will start to break down between 9 and 11 days after ovulation. This results in a drop in estrogen and progesterone levels, which causes menstruation. The luteal phase typically lasts about 14 days, but between 9 and 16 days is common.
Uterus:
Secretory Phase From ovulation until the start of the next period, The lining of the uterus releases or secretes chemicals that will either help an early pregnancy attach if an egg was fertilized, or help the lining break down and shed if no egg was fertilized
During this phase, the endometrium prepares to either support a pregnancy or to break down for menstruation. Rising levels of progesterone cause the endometrium to stop thickening and to start preparing for the potential attachment of a fertilized egg. The secretory phase gets its name because the endometrium is secreting (producing and releasing) many types of chemical messengers. The most notable of these messengers are the prostaglandins, which are secreted by endometrial cells and cause changes to other cells nearby.
Two prostaglandins in particular called, “PGF2α” and “PGE2”, cause the uterine muscle to contract (cramp). The amounts of these prostaglandins rise after ovulation and reach their peak during menstruation. The cramping caused by this prostaglandin helps trigger the period. If a pregnancy occurs, prostaglandin production is inhibited, so that these contractions won’t impact an early pregnancy. If pregnancy does not occur, the corpus luteum stops producing estrogen and progesterone. The drop in hormones, along with the effects of the prostaglandins, cause the blood vessels to constrict (tighten) and tissue of the endometrium to break down. Menstruation begins, and the whole cycle starts all over again.